
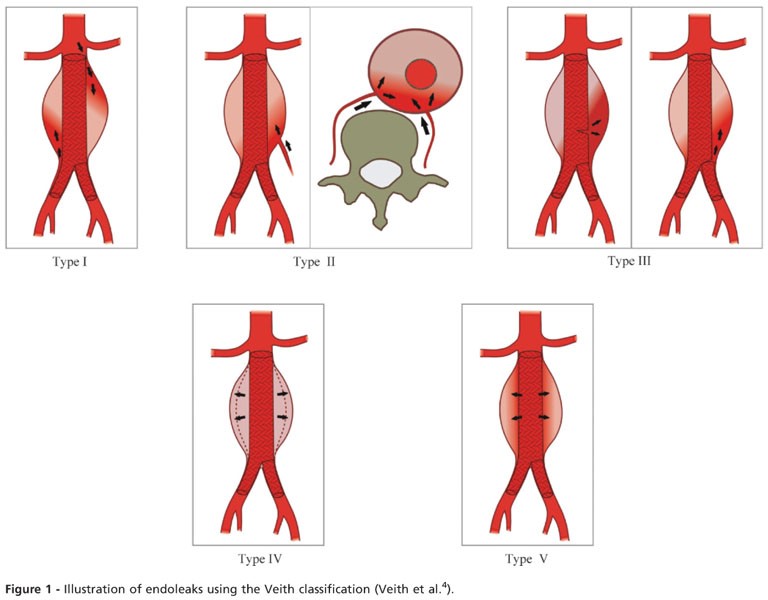
Post-operative type II endoleak is a rare but highly complex complication after PAA surgery and is extremely difficult to treat. To date, no consensus has been reached among vascular surgeons as to the best treatment for PAA, and several studies have failed to demonstrate a difference in superiority between OR and ER ( 7- 17). However, ER’s long-term follow up results remains unclear. ER is more mini-invasive when compared with OR, it only requires local anesthesia upon most occasions and needs less operation time than OR. As technology advances, the use of endovascular repair (ER) in the treatment of PAA has emerged as a potential alternative to OR. For example, OR requires general anesthesia and it needs several hours to complete the surgery, which could bring burden to patients’ respiratory and circulation system. Despite OR has definitive outcomes, it still has several disadvantages. OR produces excellent results, including good graft patency and a low limb loss rate. Since John Hunter first introduced the surgical repair of PAAs in 1795 ( 6), open repair (OR) with endoaneurysmorrhaphy and venous bypass has been the “gold standard” surgical treatment option for PAA patients. Additionally, acute lower limb ischemia leads to major amputation in 30–40% of PAA patients ( 4, 5). The 5-year complication rate is reported to be 60–75% ( 3, 4). More than half of PAA cases are asymptomatic, but PAAs can cause various complications, including acute or chronic lower limb ischemia, rupture, and major amputation.

The main causes of PAA include atherosclerosis, trauma, infection, auto-immune diseases, etc. Popliteal artery aneurysms (PAAs) are rare but account for 70–80% of peripheral artery aneurysms, and have an overall incidence of 0.01–0.1% ( 1, 2). Keywords: Popliteal artery aneurysm (PAA) open repair (OR) endovascular repair (ER) procedure approach type II endoleak However, more high-quality, large-scale randomized controlled trials need to be conducted. However, we found that autologous vein grafts have better graft patency and the posterior approach is less likely to lead to type II endoleaks and sac enlargements after the initial PAA surgical procedure. Type II endoleaks and post-operative sac enlargements were less likely to occur in OR patients when the posterior approach was adopted.Ĭonclusions: We failed to establish any difference in superiority between OR or ER. However, in the sub-group analysis, autologous vein grafts had significantly higher primary and secondary graft patency rates than expanded polytetrafluoroethylene (ePTFE) vascular grafts and stent grafts. There were no significant differences between the ER and OR groups in terms of average surgery time, 30-day mortality, peri-operative complication morbidity, post-operative type II endoleak, sac enlargement, primary and secondary graft patency, reintervention rate, and overall mortality. The ER group had a significantly lower mean length of hospital stay, blood loss volume, and aneurysm diameter than the OR group.

Results: A total of 213 PAAs of 186 patients were surgically repaired. The secondary endpoints were primary graft patency, secondary graft patency, the reintervention rate, and overall mortality.

The primary endpoints were 30-day mortality, peri-operative complication morbidity, post-operative type II endoleak, and sac- enlargement. Methods: The data of PAA patients from January 2000 to August 2020 were retrospectively collected and analyzed.
Background: This cohort study aimed to evaluate the short- and long-term outcomes of open repair (OR) and endovascular repair (ER) and identify the most suitable graft and approach for treating popliteal artery aneurysm (PAA) patients.


 0 kommentar(er)
0 kommentar(er)
